01
4 Useful Remedies for Treating Lower Back Pain
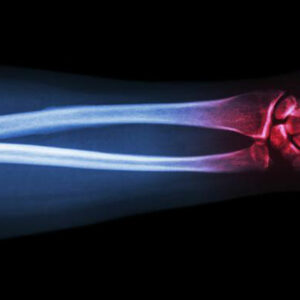
Lower back pain is a disorder involving the nerves, muscles, and bones of the back. It is a common problem that everyone suffers from at some point in their life. As the pain affects the lower end area of the spinal cord – the lumbar region, the condition is also called as lumbago. The lumbar region is a complex structure of joints, muscles, ligaments, and nerves all of which perform together to give support to the upper body. Muscles in the L1, L2, L3, L4, and L5 regions of the vertebrae are responsible for flexibility and rotation of the hips. The nerves in this area support the muscles in the limbs. If any muscles or bones are strained in this area, it can impact a person’s routine tasks. The pain symptoms can be in the form of a dull ache to a sudden stabbing sensation that can affect the body’s mobility. Daily activities like standing up straight, bending or moving around may become painful and strenuous. The condition may occur in an acute form as a repercussion of an injury or a health condition. Over time the swelling in the muscles or the nerves heal, and the pain subsides. However, if the pain extends over a few weeks, then the condition becomes chronic, and effective measures need to be taken to assuage the discomfort. Measures to ease back pain If you are suffering from pain in the lower back, here are a few ways to help reduce the distress: Rest In most instances, lower back pain can be improved by putting a break on any strenuous activity – physical or mental. Resting for a few days will take off the pressure from the lower back and allow the muscles relax. Cold and hot therapy A hot application aids in improving circulation in the afflicted area.
Read More