01
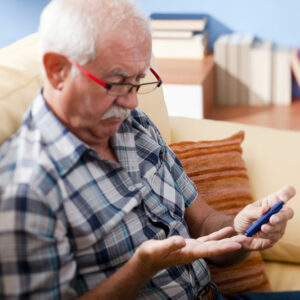
Lifestyle Changes That Can Help Control Blood Sugar
High blood sugar is a condition in which the sugar cannot be effectively transported from the blood into the cells. If left untreated, the condition can result in diabetes. As per a study, approximately 50% of the people in the country either have diabetes or are classified as pre-diabetic. Thankfully, there are some easy ways of controlling blood sugar levels to avoid all short-term and long-term problems. Here are some simple lifestyle and dietary changes to assist in diabetes. Blood sugar control measures can be taken to do that. Let’s have a look. Regular exercise Exercise is a great way to combat most illnesses. Indulging in regular exercise can help one shed off the extra weight as well as boost insulin sensitivity. This, in turn, helps the cells to better use the available sugar in the bloodstream. Also, exercise helps one’s muscles to use the blood sugar for generating energy and for muscle contraction. It is best to check blood sugar levels regularly to understand how well one’s body is responding to different activities. Controlling carb intake The body breaks down the carbs into sugar. Following that, the insulin transports this sugar into the cells. In case someone is consuming a lot of carbs or the insulin fails to properly perform its function, the entire process fails and blood sugar level spikes. So, in diabetes, blood sugar levels can be controlled by following a low-carb diet routine. This keeps the blood sugar level in check and prevents it from going up. Increasing fiber intake This is an effective way of diabetes blood sugar control. Fibers slow down the carb digestion and absorption of sugar, thus promoting a steady rise in blood sugar levels. In fact, a fiber-rich diet is known for managing type 1 diabetes. Moving on, there are two types of fibers – soluble and insoluble.
Read More 










